JACK’S HEART STORY, PART 3
If you missed Part 1, or Part 2 of our CHD Journey, be sure to check them out!
Welcome to Part 3 of our CHD Journey! In Part 2, we left off with Jack heading back to surgery. His surgery took about 5.5 hours. When the surgeon came out to talk to us, he told us a couple of things:
The left subclavian artery repair went perfectly. Blood flow to his left arm looked great and he didn’t anticipate any problems.
The vascular ring was much tighter than it had been in November when they did the bronchoscopy and CT Scan, so much that the trachea was about 85% pinched closed and obviously very inflamed. As he had shared before, the trachea is made up of soft cartilage and over time and as he grows it will repair itself. It may never be 100% open, but as it continues to heal and as Jack continues to grow, his quality of life will greatly improve and that it was unlikely he would have the wheezy breathing issues to the extent he’d had for the past 4 years.
We knew that they would determine which way to go in, once they were in the operating room after they had done another set of images. The options were either the traditional open heart down the center of his chest or a left thoracotomy. I asked the surgeon which we should hope for, he said neither. The traditional center chest open heart surgery tended to be a longer recovery, but the thoracotomy was typically a more painful recovery because of all the muscle and tissue that would be cut through. They ended up doing the left thoracotomy and inserting a chest tube.
The surgeon anticipated that Jack would be in the ICU for 2-3 days, mostly depending on the chest tube and then in a regular room for another 3-4 days before going home. They let us know that while they would not discharge us a minute before he was ready to be, that those estimations could be shortened (or lengthened) depending on his progress. Remember, this was June 2020, basically 3 months into the Coronavirus Pandemic and for a heart surgery patient (as with most patients) one of their big goals was to minimize the risk of exposure.
Once he was moved to PICU, we were able to be with him. We decided the best plan was for Sean to go back to the hotel and get some sleep, that way he could take the night shift later on.
Those first few moments walking into his PICU room were probably the hardest for me. He was starting to come out of the anesthesia and was not responding well. There were several nurses around him, holding him down because he was thrashing around so much and they didn’t want him to try to pull his chest tube out. They were so calm and said this reaction is very common, especially for young children coming out of such heavy anesthesia.
Their suggestion was to get me settled into the recliner and to get him into my lap/on my chest, almost like a newborn. The next 30 minutes were so hard, he was so disoriented and continued to thrash, scream, and cry. The nurses were so precious, they helped me hold him tight when he was thrashing around and when one of them noticed that tears were streaming down my face, she just came behind the chair and wrapped her arms around me. The Lord never stopped showing us that He was going to carry us through every single step, just as He had for the past 4 years.
After about 30 minutes, his little body had finally broken out of the anesthesia, they went ahead and gave him some pain medicine and he settled into a deep, calm sleep on my lap. I’m not sure how long he laid there, but it reminded me of those moments when he was a newborn and had fought sleep for so long , but once he finally settled, I didn’t even want to bat an eyelash for fear of waking him. Once Sean came back, we settled Jack into the bed and traded places for the night.
Day 2 was probably the hardest day. Jack was in a lot of pain from the surgery, which wasn’t surprising, but also just super uncomfortable because of the chest tube. While he loves his Daddy to pieces, he very much wanted Mommy that day and we did a lot of snuggling in his hospital bed. By the time Sean came back that evening, Jack was sitting up in the bed and even felt up to watching a little tv and eating some jello.
To my surprise, when I came into the PICU room on Day 3, they had already removed his chest tube and were getting ready to move him to a regular room on the cardiac floor. The main goals they had for us in order to be able to go home were that he was eating and drinking without throwing up, he was able to get up and walk short distances without his O2 dropping drastically and that his pain was under control with oral pain meds.
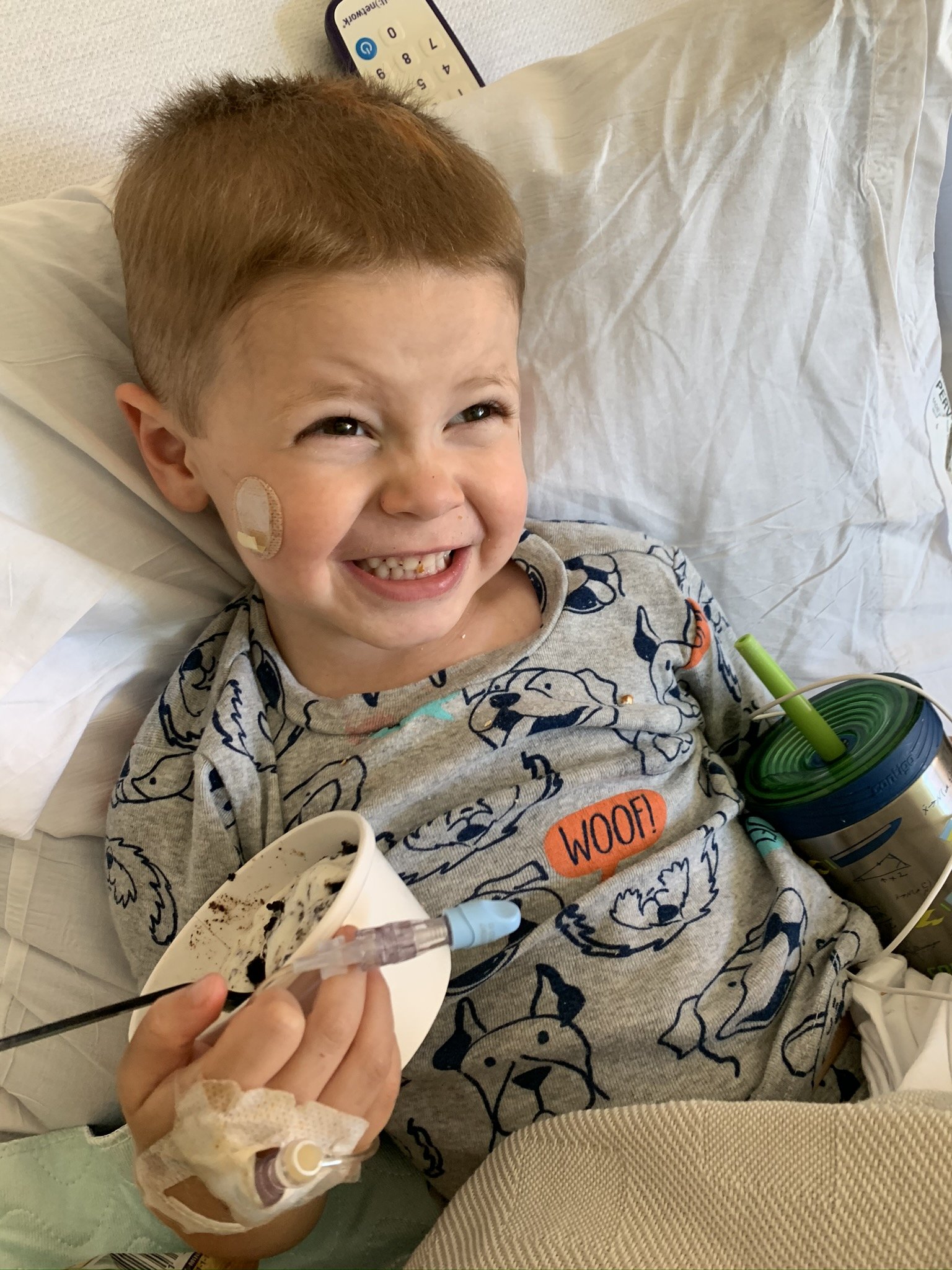
We did ALOT of snuggling, watched a lot of movies and played a lot of Kindle over the next 3 days. When our surgeon came in on Day 5 of our stay and saw that Jack had been able to walk (with me) without oxygen down to the bakery and was eating ice cream for breakfast, he gave us the green light to go home! Jack would still need to use oxygen at night until his 6-week follow-up.
I anticipated being sent home with alot of restrictions and was very surprised to hear the surgeon say, “He will guide you on his ability level. You’d be surprised at how quickly he will bounce back.” Because I knew how active my Jack Jack was prior to surgery, this was a little worrisome, but I trusted our surgeon and said let’s hit the road!
Home was just the medicine for this sweet boy. Jack was greeted by the most awesome Card My Yard display and bundles of balloons, edible arrangements and cookie deliveries from our church family. Our surgeon was exactly right, Jack really did let his body show him what he was able to do. He would play with his toys for a little bit and then ask to lay down and watch a show for a little bit. He continued to be pretty protective of his incision area for several months after surgery, but that was to be expected as the muscle tissue healed. He was only on pain medication for about a week before we were able to switch to Tylenol/Ibuprofen as needed and he continued using the Oxygen at night until his 6-week follow up.
It is amazing that something that held so much control over us for years, was corrected and healed. I was pretty worried about how his body would handle if he got sick once preschool started back up, but to our absolutely amazement he was not sick with any type of upper respiratory infections for almost a year and a half after surgery.
Jack didn’t have another upper respiratory illness until December 2021, right at Christmas. Specifically, he had Croup which targets the airway. While the fever, coughing, and runny nose all cleared up within about a week, the labored/wheezy breathing lingered for about 5 weeks. Our pediatrician and cardiologist consulted with us and both agreed that this will be a normal reaction for his body because of the anatomical differences with his trachea. They reminded me that with any type of illness, what I should look for is for his body to return to a normal baseline. For Jack, it may take 5-6 weeks for that to happen, but as he grows and his trachea continues to heal, that time should become less and less.
Today, I can report with complete and total joy that Jack is a normal, happy, silly and ENERGETIC 7 (almost 8) year old boy and he is THRIVING in second grade. We can do nothing but give the praise to Jesus. I truly believe that it was the Lord that kept that still small voice in the back of my head to continue to push for answers, it was the Lord who led us to our amazing Pediatric Cardiovascular Surgeon and it was the Lord who paved the way for Jack to have this much needed surgery in the beginning of a global pandemic.
If you have hung with me this long, thank you! Thank you for listening to and sharing our story. My greatest prayer is that Jack’s story would bring awareness to undiagnosed congenital heart defects and be an encouragement to anyone on a hard journey that the Lord will walk each and every step of that journey with you.